
9, 10, 13, 14 In our cohort, 16% of the cases were managed with a PD procedure. Despite evidence that PR is safe, many surgeons still opt to perform a PD for a number of indications. The management of destructive colonic injuries remains contentious. Septic wound complications remain common, occurring in 9% of our cases. This reflects systems failure and attention must be paid to ensuring that the appropriate levels of staff are involved in the management of these injuries. 5, 6, 8 Inexperienced staff managing complex injuries will result in poor outcomes. Of concern is the association with technical failure and/or poor patient selection and anastomotic breakdown in our series. Our anastomotic complication rate of 4% is in keeping with other reported rates. The literature over the last three decades suggests that PR of simple colonic injuries is a safe strategy and our experience supports this.
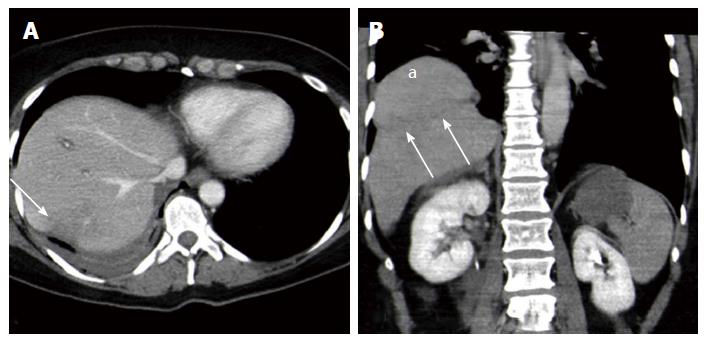
#BLUNT INJURY TO THE HEPATIC FLEXTURE SERIES#
The vast majority of injuries in this series were secondary to penetrating trauma and blunt injury cases remain uncommon. There was no significant difference in mean base excess by wound complication status ( p=0.405) and no significant difference in mean delay by wound complication ( p=0.428). In the 11 patients who developed colon related wound sepsis, there was a higher rate of anastomotic failure but this was not statistically significant ( p=0.351). There was no significant difference in mean delay between cases with breakdown and those without ( p=0.231). Systemic hypotension was defined as a systolic blood pressure of 6 hours between injury and surgery. The other three cases of anastomotic failure occurred with left-sided colonic injuries. In both of these cases, technical failure was considered to be a factor in the development of the complication. Of the five patients who experienced anastomotic breakdown, only two had sustained a right-sided colonic injury.
Individual case review identified a number of risk factors for anastomotic failure, which included technical error ( n=2) and PR in the presence of clear indications for DC surgery ( n=2).

The purpose of this study was to audit our current management and outcomes of colonic trauma, to review our experience of colonic trauma in patients who underwent DC surgery and to produce a clinical algorithm for assisting with the management of these injuries.
#BLUNT INJURY TO THE HEPATIC FLEXTURE HOW TO#
18– 24 The controversies in colonic trauma revolve currently around management of destructive colonic injuries, initial selection of cases for DC and (once a DC approach has been chosen) how to manage colonic injuries that have been temporised during the initial procedure.
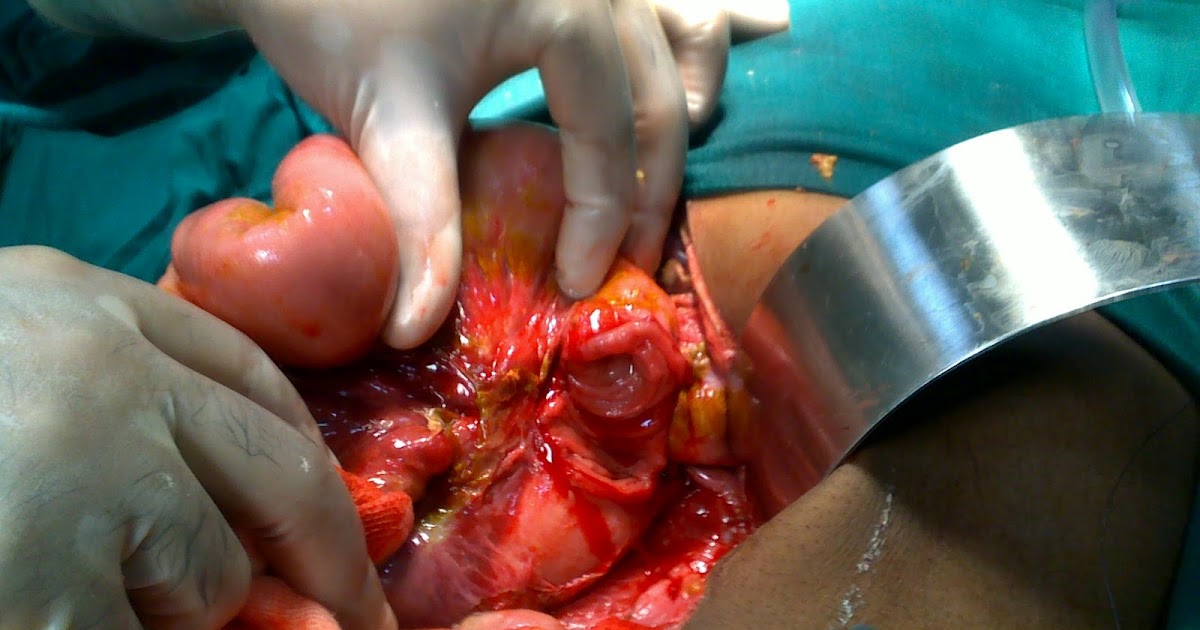
The principle of DC is to avoid all definitive surgery in the unstable patient at the initial operation, and to control bleeding and soiling in an abbreviated procedure. The emergence of damage control (DC) surgery towards the end of the 20th century once again changed the debate about primary colonic repair. Management of destructive colonic injuries still appears to be highly individualised. 13– 17 Several authors, however, have reported fairly large series of civilian colonic GSWs that were managed successfully by PR. The two situations where it was initially thought diversion would be required were civilians with a colonic gunshot wound (GSW) and patients with destructive colonic injuries. 13– 15 The debate changed from which cases should be managed with PR of a colonic injury to which subgroups of patients still required a diversion. 3– 10, 12 The pendulum of surgical opinion swung increasingly away from mandatory diversion towards a policy of almost universal PR. 1, 2 This dogma has been challenged since the last quarter of the 20th century as authors began to publish their experience with either exteriorised repair or selective primary repair (PR) of civilian colonic injuries. 1– 12 Following the experience of military surgeons during the Second World War, mandatory diversion of all colonic injuries became the standard of care in civilian practice.
Management algorithms for colonic trauma have evolved over the last few decades.


 0 kommentar(er)
0 kommentar(er)
